
In summary:
- Chronic arthritis pain can be managed by moving beyond passive pill-taking to a proactive, holistic approach.
- Effective strategies include targeted physical therapies (heat/cold, TENS), significant dietary changes to reduce inflammation, and safe, joint-friendly exercise.
- Understanding the risks of medication, such as dependency and the “prescribing cascade,” is crucial for long-term health.
- True relief involves becoming an active partner in your healthcare, including having informed conversations with your doctor about reducing medication.
Living with chronic arthritis often feels like a constant negotiation with pain. For many, the default response handed down has been a prescription pad, leading to a cabinet filled with painkillers that promise relief but often come with a host of side effects and anxieties. You take one pill for the pain, another for the side effects of the first, and soon feel trapped in a cycle that manages symptoms but never addresses the root cause or empowers you.
The common advice to “eat healthy” or “get some exercise” feels vague and unhelpful when every movement hurts. It’s easy to become discouraged, feeling as though your only options are to endure the pain or accept the risks of long-term medication use. This feeling of being stuck is a heavy burden, one that can diminish your quality of life far more than the joint pain itself.
But what if the path to meaningful relief isn’t found in a new pill, but in a new perspective? The key is to shift from being a passive recipient of treatment to the active architect of your own well-being. This involves developing a deeper “body literacy”—learning to understand the signals your body is sending and responding with targeted, non-pharmacological strategies. It’s about treating the system, not just the symptom.
This guide is designed to empower you with that knowledge. We will explore effective, evidence-based methods for managing arthritis pain that go beyond medication. From understanding the science of heat therapy to learning how to talk to your doctor about deprescribing, you will gain the tools to build a comprehensive pain management plan that puts you back in control.
To help you navigate these powerful strategies, this article is structured to guide you step-by-step, from immediate physical therapies to long-term lifestyle adjustments and crucial conversations with your healthcare provider. Below is a summary of the key areas we will explore.
Summary: A Holistic Path to Arthritis Pain Management
- Heat vs Cold: which therapy actually works for osteoarthritis flare-ups?
- How to use a TENS unit at home to block pain signals effectively?
- Why sugar and processed foods might be doubling your joint pain?
- The opioid trap: signs you are developing a dependency on pain meds
- Turmeric vs Ibuprofen: comparing natural and pharmaceutical anti-inflammatories
- Why taking a pill to treat the side effect of another pill is a dangerous cycle?
- How to perform resistance training without straining arthritic joints?
- Effective Pharmacotherapy: How to Start the Conversation About Deprescribing with Your Doctor?
Heat vs Cold: which therapy actually works for osteoarthritis flare-ups?
One of the most accessible and immediate ways to manage arthritis pain is through thermotherapy—the strategic application of heat or cold. However, using the wrong one at the wrong time can be ineffective or even counterproductive. Understanding the ‘why’ behind each method is the first step in building your personal pain architecture. It’s about listening to your body and giving it what it needs in the moment.
Heat therapy, such as a warm compress, heating pad, or a warm bath, works by increasing blood flow to the affected area. This vasodilation helps relax tight muscles, decrease stiffness, and soothe the chronic ache that often settles into joints. It’s best used for the persistent, non-swollen stiffness you might feel in the morning or after a period of inactivity. For maximum benefit, you can apply moist heat for 15-20 minutes, two to three times a day, to help lubricate the joints and improve your range of motion before gentle activity.
Conversely, cold therapy (cryotherapy) is your tool for acute flare-ups characterized by inflammation, swelling, and sharp pain. Cold packs or ice baths cause vasoconstriction, which narrows blood vessels. This process numbs the area, providing immediate pain relief, and more importantly, reduces the inflammatory response that causes swelling and joint damage. Apply a cold pack wrapped in a towel for no more than 15 minutes at a time to avoid skin damage, taking breaks of at least 30 minutes between applications. Think of cold as the emergency response for a “hot” and angry joint.
In some cases, a contrast therapy, alternating between hot and cold, can be beneficial for stimulating circulation and reducing stiffness without increasing inflammation. The key is to develop your body literacy: use heat for stiffness and chronic ache, and cold for acute inflammation and swelling.
How to use a TENS unit at home to block pain signals effectively?
Beyond simple temperature changes, technology offers another powerful, non-invasive tool for your pain management toolkit: the TENS unit. TENS, or Transcutaneous Electrical Nerve Stimulation, might sound intimidating, but it is a safe and widely used method for controlling pain at home. It works on a simple principle: if you can intercept the pain message before it reaches the brain, you don’t perceive the pain. It’s a way of closing the “gate” on pain signals.
A TENS unit is a small, portable device connected to electrodes that you place on your skin around the painful joint. When activated, it sends a mild, tingling electrical current through the skin. According to guidelines for managing arthritis pain, this current does two things. First, it stimulates non-pain sensory nerves, which effectively “busies” the nerve pathways to the brain, blocking the slower-traveling pain signals from getting through (the “Gate Control Theory”). Second, it can trigger the body’s release of endorphins, our natural painkillers.
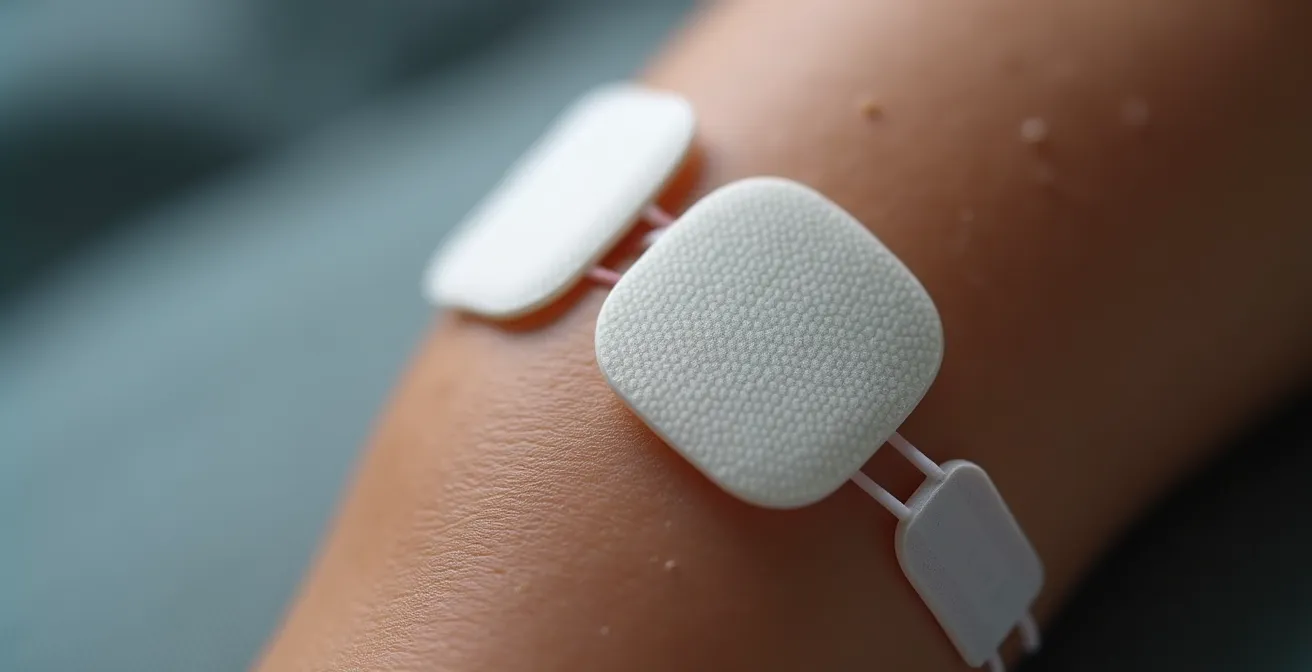
For effective home use, it’s about finding the right settings and placement. You should start with a conventional high-frequency setting (around 80-100 Hz) for 30-40 minutes at a time. The sensation should be a strong but comfortable tingling, not painful or causing muscle twitches. You can experiment with placing the electrode pads on either side of the painful joint, above and below it, or directly over the most tender points. The goal is to find the placement that provides the most significant reduction in your perceived pain. It’s a prime example of proactive self-management, allowing you to have a pain-relief tool on demand, without a pill.
Why sugar and processed foods might be doubling your joint pain?
While external therapies like heat and TENS units manage pain signals, what you put inside your body can either fuel the fire of inflammation or help to extinguish it. Many people with arthritis are unaware that their diet may be a primary driver of their pain levels. The link is clear: certain foods, particularly added sugars and highly processed products, promote a state of systemic, low-grade inflammation throughout the body, which can dramatically worsen joint pain and stiffness.
When you consume refined sugars, trans fats, and processed carbohydrates, your body can respond by releasing inflammatory messengers called cytokines. For someone with arthritis, whose immune system is already prone to an inflammatory response, this is like pouring gasoline on a smoldering fire. The result is increased swelling, stiffness, and pain in the joints. This isn’t about a single “bad” meal, but rather a cumulative effect where a consistently pro-inflammatory diet keeps your body in a constant state of alert, exacerbating your arthritis symptoms day after day.
Conversely, adopting an anti-inflammatory diet rich in whole foods can have a profound effect. This means focusing on fruits, vegetables (especially leafy greens), healthy fats (like those in olive oil, avocados, and nuts), and fatty fish rich in omega-3s. These foods contain antioxidants and other compounds that actively combat inflammation. The process of identifying your personal trigger foods is a crucial part of developing body literacy. What causes a flare-up in one person may not affect another, making a systematic approach essential.
Your 2-Week Inflammation Elimination Protocol
- Weeks 1-2: Eliminate all added sugars, processed foods (anything in a box with a long ingredient list), and refined carbohydrates like white bread and pasta.
- Daily Fuel: Actively add 3-4 servings of potent anti-inflammatory foods like berries, leafy greens, walnuts, or fatty fish (e.g., salmon).
- Pain Journal: Track your pain, stiffness, and energy levels each morning and evening on a simple scale of 1-10 to create a baseline.
- Systematic Reintroduction: On Week 3, reintroduce ONE food group you eliminated (e.g., dairy or wheat) and monitor your pain journal for any changes over the next 48 hours.
- Identify Triggers: Through this careful process, you can pinpoint your personal “trigger foods” and build a sustainable, pain-reducing diet.
The opioid trap: signs you are developing a dependency on pain meds
While non-drug strategies form the foundation of holistic pain management, pharmacotherapy has its place. The danger, however, lies in the slow, often unnoticed slide from appropriate use to dependency, particularly with opioid painkillers. The “opioid trap” doesn’t snap shut overnight; it’s a gradual process where the medication starts to control you, rather than the other way around. Recognizing the early warning signs is critical to avoiding this dangerous path and maintaining control over your health.
Dependency often begins with a subtle psychological shift. You may start “pain-chasing”—taking a pill in *anticipation* of pain before an activity, rather than in response to actual pain. Your tolerance can increase, meaning you need a higher dose to achieve the same level of relief you once got from a smaller amount. This dose escalation, especially when done without consulting your doctor, is a major red flag. Your focus may narrow, and you might feel a rising sense of anxiety or panic when you realize your prescription is running low or you’ve misplaced your pills.
Another tell-tale sign is when the medication’s purpose begins to blur. You might find yourself reaching for a painkiller not just for joint pain, but to manage stress, to help you sleep, or to lift your mood. The pill becomes a crutch for emotional as well as physical discomfort. If you’ve tried to cut back on your own but found the increase in physical pain or emotional distress unbearable, it’s a strong indicator that a dependency has formed. Acknowledging these signs isn’t a moral failing; it’s a crucial act of self-awareness and empowerment.
To help you reflect honestly, consider the following questions:
- Do you find yourself taking medication in anticipation of pain rather than in response to it?
- Have you increased your dose over time without discussing it with your doctor?
- Do you feel anxious or preoccupied when your medication supply is running low?
- Have you tried to reduce your intake but experienced a significant increase in pain or emotional discomfort?
- Are you using the medication for reasons other than physical pain, such as to cope with stress or to help you sleep?
Turmeric vs Ibuprofen: comparing natural and pharmaceutical anti-inflammatories
In the quest to manage inflammation, many people find themselves at a crossroads: should they rely on a proven pharmaceutical like ibuprofen or explore a natural alternative like turmeric? This isn’t an “either/or” choice but a strategic one. Understanding the distinct mechanisms, benefits, and limitations of each allows you to use them intelligently as part of your overall pain architecture—one for acute attacks, the other for long-term maintenance.
Ibuprofen is a non-steroidal anti-inflammatory drug (NSAID) that works by inhibiting COX enzymes, which are key players in the inflammatory cascade. It’s highly effective and fast-acting, providing relief from acute flare-ups within an hour. However, its long-term use is associated with significant risks, including gastrointestinal issues like ulcers, and an increased risk of cardiovascular problems. It is a powerful tool for short-term, rescue relief but a problematic solution for daily, chronic management.
Turmeric, on the other hand, contains an active compound called curcumin, which works differently. Instead of blocking a single pathway, it modulates multiple inflammatory pathways in the body. Its effect is more systemic and less immediate, often taking several weeks of consistent use to build up and notice a difference. Its major advantage is a much lower risk of side effects. The key challenge with curcumin is bioavailability—it’s poorly absorbed by the body. However, studies demonstrate that turmeric absorption increases by up to 2000% when it’s combined with piperine, the active compound in black pepper. This makes supplementation or dietary use far more effective.

| Aspect | Turmeric/Curcumin | Ibuprofen |
|---|---|---|
| Mechanism | Modulates multiple inflammatory pathways (NF-κB) | Non-selective COX inhibitor |
| Time to Effect | Several weeks of consistent use | Within 1 hour |
| Side Effects | Minimal when taken with food | GI issues, cardiovascular risks with long-term use |
| Best Use | Daily maintenance, long-term inflammation reduction | Acute flare-ups, short-term relief |
Why taking a pill to treat the side effect of another pill is a dangerous cycle?
One of the most insidious risks of a medication-heavy approach to chronic illness is the “prescribing cascade.” This dangerous cycle begins when a side effect from one drug is misinterpreted as a new medical condition, leading to the prescription of a second drug to treat it. This can trigger a domino effect, adding more medications, more side effects, and more complexity, all while moving further away from addressing the original problem. For seniors with arthritis, this is an especially common and hazardous trap.
The prescribing cascade buries the root cause under layers of new symptoms and treatments, making it difficult for both you and your doctor to see the full picture. It increases the risk of adverse drug reactions, drains your energy, and can lead to a sense of being perpetually unwell, even when your primary condition is stable. Breaking this cycle requires a fundamental shift from a “symptom vs. system” mindset to one of active medication partnership and vigilance.
Case Study: The Common Arthritis Prescribing Cascade
A classic example of this cascade, highlighted in research on medication management, often starts with arthritis pain. Step 1: A patient is prescribed a high dose of an NSAID (like ibuprofen) for joint pain. Step 2: The NSAID causes acid reflux and stomach upset as a side effect. This is misinterpreted as a new diagnosis of GERD. Step 3: A Proton-Pump Inhibitor (PPI) is prescribed to treat the reflux. Step 4: Long-term use of the PPI depletes the body’s magnesium and Vitamin B12. Step 5: This deficiency leads to new symptoms like fatigue, muscle cramps, and neuropathy, which may trigger yet another round of diagnoses and prescriptions. The original issue—arthritis pain—is now buried under a mountain of medication-induced problems.
Escaping this cascade begins with a simple but powerful question you should ask at every medical appointment where a new symptom is discussed: “Could this be a side effect of a medication I’m already taking?” This single question can reframe the entire conversation, prompting a medication review rather than a new prescription. It is the cornerstone of safe and effective pharmacotherapy, transforming you from a passive recipient into a vigilant guardian of your own health.
How to perform resistance training without straining arthritic joints?
For many with arthritis, the idea of “resistance training” conjures images of heavy weights and painful movements, leading them to avoid it altogether. This is a critical mistake. When done correctly, building muscle is one of the most effective long-term strategies for protecting your joints and reducing pain. Strong muscles act as natural shock absorbers, taking pressure off the cartilage and bone. The goal isn’t to become a bodybuilder, but to create a supportive muscular framework around your vulnerable joints.
The connection between muscle strength, weight, and joint pressure is direct and profound. As an example, research demonstrates that for every one pound of weight you lose, you remove four pounds of pressure from your knee joints. Building muscle helps you achieve and maintain a healthy weight by boosting your metabolism, creating a virtuous cycle of less pressure and less pain. The key is to choose the right kind of exercise that builds strength without causing a flare-up.
One of the safest and most effective methods is isometric exercise. Unlike traditional weightlifting (isotonic exercise), which involves moving a joint through its range of motion, isometrics involve contracting a muscle without any joint movement. This allows you to strengthen the muscles that support a joint without actually stressing the joint itself. For example, to strengthen your quadriceps to support a painful knee, you could sit in a chair, extend your leg straight, and simply tighten the thigh muscle, holding the contraction for 10 seconds before relaxing. This can be repeated for several sets.
Physical therapy studies show that patients who perform daily isometric holds for major muscle groups around their arthritic joints report significantly improved joint stability and reduced pain within just 4-6 weeks. Other low-impact options include water aerobics, where the buoyancy of the water supports your body weight, and using resistance bands, which provide gentle, controlled resistance. The focus is always on slow, controlled movements and stopping immediately if you feel any sharp pain.
Key Takeaways
- True pain management is an active process of building a personalized plan, not passively taking pills.
- Combining physical therapies, anti-inflammatory nutrition, and safe exercise creates a powerful, synergistic effect.
- Vigilance about medication side effects and a collaborative partnership with your doctor are essential for long-term safety and well-being.
Effective Pharmacotherapy: How to Start the Conversation About Deprescribing with Your Doctor?
After building a strong foundation of non-pharmacological strategies, the final and most empowering step is to approach your medication list with a critical eye. This is known as “deprescribing”—the planned and supervised process of reducing or stopping medications that may no longer be necessary or may be causing harm. This is not something to do on your own. It requires a strong medication partnership with your doctor, transforming your relationship from a passive one to a collaborative one focused on your overall quality of life.
The key to a successful conversation is to frame it around your functional goals, not just pain. Instead of saying “I want to stop this pill,” try focusing on what you want to achieve. This shifts the conversation from one of subtraction to one of positive ambition. Your doctor wants to help you live a fuller life, and aligning your medication plan with that goal is a powerful motivator for them as well.

Walking into the appointment prepared is crucial. Schedule a specific appointment just to review your medications, so it doesn’t get rushed at the end of a regular visit. Bring a complete list of everything you take—prescriptions, over-the-counter drugs, vitamins, and supplements. Having a simple script prepared can also help you overcome any hesitation. For instance, a clear, goal-oriented statement can open the door to a productive dialogue. As suggested by pain management guidelines, you could start the conversation like this:
Doctor, my goal is to be more active. I’d like to explore if we can create a plan to optimize my medications to help me achieve that, perhaps by reducing any that are no longer essential.
– Suggested script, Managing Arthritis Pain Guidelines
This approach establishes you as a proactive partner. From there, you can ask targeted questions like, “What is the minimum effective dose for my condition?” or “Can we create a gradual tapering plan with regular check-ins?” This process is the ultimate expression of taking control—not by rejecting medicine, but by mastering it in partnership with your trusted provider.
By applying these holistic strategies and fostering an open dialogue with your healthcare team, you can move beyond simply managing pain and begin to truly architect a life of greater comfort, mobility, and control. Start today by choosing one strategy to implement and schedule that crucial medication review appointment.
